The suggestion of a COPD patient using fasting as a tool to manage their disease will raise the odd eye brow. However, the many benefits of fasting would indicate it being a worthwhile strategy to explore for respiratory patients.
What is fasting?
Fasting is consuming no calories over a set period of time, it can be carried out in a number of ways. Water fast, fat fast, intermittent fast and prolonged fasts just to name a few. For the point of this blog post we’ll discuss a prolonged water fast as this is the one I have just completed.
The aim of fasting is to take little to no calories in for the period you’re fasting. Some of the benefits of fasting include weight loss, reducing oxidative stress, rejuvenating stem cells in the immune system, reducing blood/glucose and insulin levels. The main benefit of fasting I’m interested in is the suppression of inflammation.
The study
At this time, there has been no studies into the benefits of a fasting protocol for COPD patients which I’m aware of. While fasting is not for everyone, there is a population of patients, myself being one of them, which are relatively stable patients in a healthy weight range. This could well be the ideal study group, as adapting to a fasting protocol would not be terribly difficult.
In today’s world, if you can’t bottle it and sell it, there will be little interest in studying it. If fasting or nutritional strategies are to become widely used then I suspect it will be driven by patient experience rather than large expensive studies.
I recently completed a 5 day fast which consisted of water, green tea and bone broth. Carrying out a 5 day fast cold turkey is not something I’d recommend as the first 2 days may be hard to get through. My fasting plan was to consume at least 2lts of water per day and using green tea and bone broth as I needed.
Bone broth can provide your body with valuable minerals while fasting, including magnesium, calcium, potassium. Green tea has zero calories as well as great antioxidant properties.
I have been using a ketogenic diet for nine months. This diet mimics some of the effects of fasting. My decision to take part in a five day fast was more for the effects on inflammation and the rejuvenation of my immune system which has taken a beating over the last 3 months. I contracted a nasty chest infection whilst overseas earlier in the year which lead to the most severe exacerbation I have experienced since diagnosis. Basically, I was willing to try anything in order to feel a little better.
The fast
Being on the ketogenic diet gave me a good foundation to completing the fast due to the low amounts of carbohydrates I consume daily. Also, I generally only eat only 1-2 meals per day. I have also incorporated a 24 hour fast once a week into my nutrition strategies.
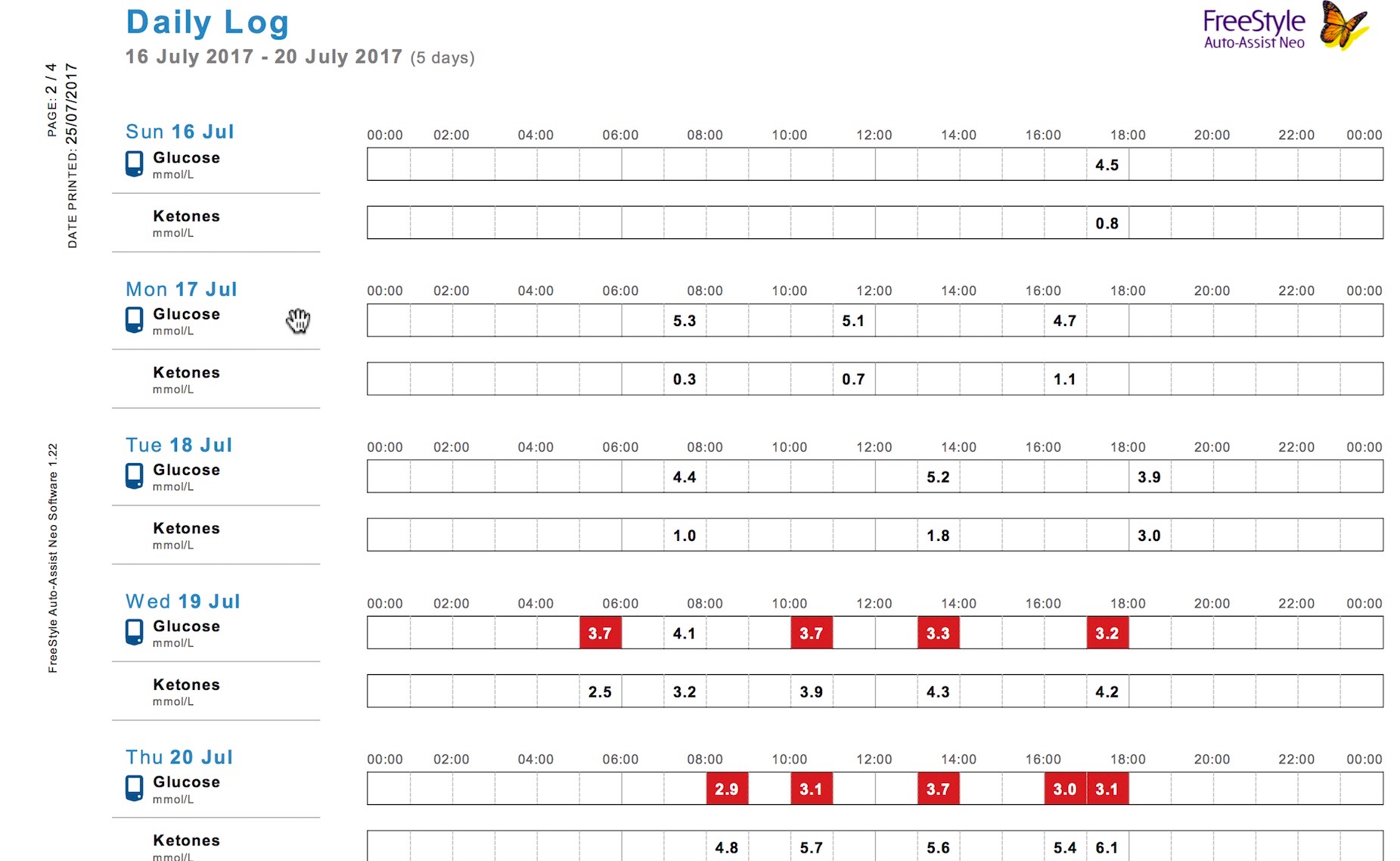
The first 2 days can be the toughest as your body depletes itself of glucose and converts over to using ketone bodies as fuel. Due to being already adapted to ketones I had no problem as my glucose levels were fairly low at the start of this fast.
My first four days were uneventful as I didn’t have hunger pains and life went on as normal. I completed a gym session on day three and walked every day. I think it’s important to keep busy while fasting so you’re not thinking about food.
By day 5 I had noticed a boost in energy, this increase in energy correlated with my high ketone levels. What surprised me about this fast was the longer the fast lasted the more I was thinking I could go another 2 or 3 days easily.
Unfortunately, I was not able to record my spirometry over the fast but I did monitor my oxygen levels, which remained above 96%. I did not notice any difference with my breathing in the first 3 days, however day 4 and 5 I felt less laboured in my breathing. I’m not a scientist but I do know the less inflammation in my airways, the easier it is to breathe
What I hope to find
I had a range of blood test toward the end of the fast which will cover such things as inflammation markers, insulin levels and general blood examination. What I hope to see is suppressed inflammation and insulin levels with other blood markers being in a normal range.
At the time of publishing this article I can report on two results. C- Reactive protein levels are <5. CRP is a marker of inflammation, many COPD patients have very high levels of inflammation. Fasting insulin is 2 mU/L which is well within the accepted range of <25.


So far so good, I’m looking forward to seeing the cytokine blood panels when they are back. Stay tuned for my follow up article and review on all of my fasting tests.
Thanks for keeping an active participation of your own care! I would be interested in the effect the fasting has on your pCO2. I do understand the inflammation control you are trying to determine, but if, during the inflammatory incidents, your arterial blood gas level may have increased causing an increased workload for your body. Just an added parameter to prove the level of improvement you experience with the fast.
If you Google COPD fasting the first result will be that of a study: https://www.ncbi.nlm.nih.gov/pubmed/23265268
If you Google COPD fasting the first result will be that of a study: https://www.ncbi.nlm.nih.gov/pubmed/23265268
I’m looking for a follow up! When do you plan on writing it?
Oh, and btw. you can fast for as long as you feel like it. When you start feeling hungry again that’s the cue to get back to eating.
Here are few videos on the subject (the rest of the channel has some good ones as well):
https://www.youtube.com/watch?v=APZCfmgzoS0
https://www.youtube.com/watch?v=Dan8qtgQRi8
https://www.youtube.com/watch?v=zcMBm-UVdII
Just to be clear, these are not my videos – I’m just providing them as they are relevant.
Did you experiment with GAPS protocol or the like? Also did you had experience with any of these; Beta Glucan, CoQ10 (Ubiquinol), N-Acetyl-l-Cysteine, Omega-3 (preferably with Krill and Astazanthin), good probiotic. Supposedly they can be rather helpful in some cases of COPD.
Cheers,
Dan
Hi Russell
What is your latest views on water fasting for COPD. I do regular 5 day water fasts and see a reduction in my cough and lung inflammation. Fasting also appears to improve my immune system hence making me less prone to exarcerbations.
Interested to hear if other people also use fasting as part of their disease management approach and their experiences.
Hi David. I think fasting or a fasting mimicking diet as promoted by Dr Volta Longo will be a strategy for managing COPD into the future. It has worked for me and I continue to use intermittent fasting as part of my strategy.
Just diagnosed with “mild” COPD. I’ve read Dr. Longo and about fasting mimicking diets. Have you studied/experimented in this area since you wrote about this subject several years ago? I would be interested if there is any further progress on using fasting for COPD.
David have you experimented further on fasting for COPD? I would be interested in any updates!
Wouldn’t expect the reader to believe what follows, but Angus Barbieri … PROBABLY … holds the world record for fasting at 382 days. From the Wikepedia article, entitled “Maryfield Hospital:”
“In the 1960s a world record was set at the hospital when a patient named Angus Barbieri spent 382 days between June 1965 and July 1966 without taking solid food. Barbieri survived by taking tea, coffee and soda water as well as vitamins.[7][8] During that period, his weight declined from 214 to 80.74 kilograms (33 st 9.8 lb to 12 st 10.0 lb; 471.8 to 178.0 lb).”
Hi Alan, I am familiar with this story, amazing!
I’m so glad that I found this Since alternately I am looking for a cure Rather than just managing the issue. I am overweight and intend to use The fasting to lose out excess weight Not undergo unnecessary stress to my body while doing so
Is this effective for those who have advanced COPD?
Hi Cristal. Personally I would say yes. I am classified as a very severe patient and it works for me. If your unsure talk to a dietician who has experience with the ketogenic diet. This is also a great resource – https://www.ketonutrition.org
Best,
Russell
Do you use oxygen at all?
Yes, when at altitude and when I exercise.
Hi I do keto and been intermittent fasting for awhile now and was 243lbs. when I started keto after only 3 months went to 205 lbs, I do believe that this can cure copd I am stage 3 right now, I just did a 2 1.2 day dry fast and only ended it cause I did not prepare properly and was constipated and did not want complications so ended it early. I honestly think if I can do enough dry fasts in a row with a short water fast in between I can cure myself from Autophagy and my own stem cells.
I am not a doctor nor do I have any training but I feel this is a fact and the only true cure other than a cloned lung replacement.
longest water fast I did was 13 days, I plan to try and do some more tests soon….. and thoughts out there…. I am going to be 65 this Feb. look forward to hearing your thoughts and if you know anyone who would be interested in doing a study and wants a subject to help them out I would be glad to but I can not travel or pay since I am on limited income and can not drive.
There is no evidence at this stage which shows regeneration of stem cells through fasting can help with lung disease. Thats not to say it can’t. I’m not aware of anyone doing those studies and given the lack of research dollars for COPD, its unlikely to happen any time soon. keep me posted on your progress.
I too am turning 65 with copd and very interested in a fasting buddy
I’ve had two hospitalizations for copd and just recently qualified for at home oxygen. I literally had issues walking across my house and conducting daily skills. I’m morbidly obese. I’ve just started one meal a day and I instantly had energy, feel better overall and can manage daily skills. My pulse ox which normally is <90, has increased. I feel motivated that using fasting will help me lose weight and in turn increase my ability to breathe. I for the first time in two years feel better, emotionally hopeful and less anxious/depressed.
Great to hear Judy, keep me posted on your progress.
I definitely feel fasting helped my copd. Last year I did a 12 day water fast. Yes, first 2 days were the hardest, so for those 2 days I had 8oz of broth in the evening. After that I didn’t need it. I continued my supplements, because I also have MS and can’t do without my vitD & B12, but not on disease modifying. Many days I forgot to do my Spiriva & didn’t need my emergency inhaler at all. The only reason I stopped was because my mouth wanted to chew. Looking back, I should’ve just chewed & spit out. Planning to do another because I’m recently recovering from a chest cold and believe it will help. I only lost 5 lbs and I put that down to my hypothyroidism. Good luck everyone.